Grade: Excellent
The ketogenic diet induces ketosis and that’s a good thing because ketosis brings with it a raft of health benefits. It’s a diet in the sense that what you eat is important, but how much you eat isn’t that important. Also there’s the whole weight loss thing, but that’s more of a side note. The importance of this diet lies in its mechanisms to prevent and possibly even treat Alzheimer’s.
Moving from Glycolysis to Ketosis
Most diets include a high percentage of simple carbs (bread, rice, pasta, etc.). Those carbs along with sugar (in all its forms) are quickly converted to glucose. This glucose is stored in the liver as glycogen and the rest used by mitochondria as the substrate for making energy. This assumes that one is not eating excessive amounts of carbs and sugar as that would produce chronic stress on the system and lead to weight gain on the way to full blown diabetes.
The ketogenic diet is high in fat and has few or even zero carbs. In response to the lack of dietary glucose, the body taps the glycogen stored in the liver to make glucose. When the glycogen reserve is depleted the body turns to creating the minimum amount of needed glucose from proteins and fats. The liver is then free to crank out ketone bodies (ketones) from fatty acids. These ketones (primarily beta-hydroxybutyrate) are used by mitochondria to produce energy. Congratulations you are now in ketosis.
Ketosis versus Alzheimer’s
The ketones produced by the liver from dietary fat and other sources become the primary fuel for our cells. As we will see mitochondria respond by producing more energy and fewer ROS, fatty deposits shrink, blood pressure goes down, inflammation is tamped down, mood stabilizes, amyloid-beta and tau tangles are cleared, oxidative stress is avoided, and new neurons and mitochondria are created. In short, the steady march of Alzheimer’s is reduced to a shuffling gait.
Ketones help Mitochondria
Mitochondria can produce more ATP with ketones. Ketones are a more efficient source of energy per unit oxygen than glucose producing 129 molecules of ATP per molecule of fat versus 36 molecules of ATP from a molecule of glucose. In addition to the extra energy production, our brain cells have an easier time using ketones perhaps because glucose metabolism in the brain becomes less efficient as we age.
Mitochondrial produce fewer ROS with ketones. Reactive oxygen species (ROS) get a bad rap, but are a normal byproduct of several cellular functions and are important to cell signaling. When all is going well they are like an alarm clock. When all hell breaks loose they are like a emergency siren because chronic elevated ROS triggers apoptosis also known as the cell’s self-destruct sequence.
Ketones are not themselves anti-oxidants, rather ketones produce cellular efficiencies that reduce the production of ROS. Already mentioned is the upregulation of BDNF that enhances the creation of new mitochondria (the more the merrier). Also involved in ROS reduction is the enhancement of NAD ratios (necessary for efficient oxidation during ATP production) and enhanced mitochondrial respiration. All of the above was accomplished without increases in the naturally produced antioxidant glutathione, further indicating reduced ROS production as opposed to additional mopping up of excess ROS.
Ketones Disrupt Inflammation by Preventing Glutamate Excitotoxicity
Ketones reduce glutamate and aspartate levels. Aspartate and especially glutamate latch onto the NMDA receptor and excite it into producing more glutamate. Over-excitation results in bad feedback loops of inflammation that are damaging to neurons (see QUIN is not your friend: Quinolinic Acid and Alzheimer’s for more details). A study of cerebrospinal fluid amino acids in 26 children on the ketogenic diet showed reductions in both aspartate and glutamate. Ketones even prevented mitochondria from succumbing to glutamate induced exitotoxicity.
Ketones increase GABA. GABA also binds to the NMDA receptor, but with the opposite effect. It has a calming effect and therefore curtails production of glutamate. Ketone bodies have been found to increase brain synaptosomal GABA content.
Ketones switch a key metabolic pathway to producing Kynurenic acid (KYNA) KYNA is another calming NMDA receptor antagonist and KYNA levels are increased in ketosis by substantial amounts. Compared to rats fed a regular diet, the ketogenic diet resulted in an increase of KYNA concentrations in the hippocampus of 256% for young rats and 363% for adult rats. The increases in the striatum were 381% for young rats and 191% for adult rats.
Ketones reduce blood pressure. High blood pressure can force pathogens past the blood brain barrier and Alzheimer’s patients often have a leaky blood brain barrier. Furthermore, bacterial loads in Alzheimer’s brains are usually higher. Cause and effect are hard to determine, but correlation is high. Regardless, lowering blood pressure is an all around health benefit.
Ketones disrupt metabolic disorder. If you are in ketosis you are not consuming excess sugar and carbs and your insulin levels will remain low. When insulin levels are low the body has the resources to degrade amyloid-beta plagues. Finally, diabetes is highly correlated with Alzheimer’s.
Ketones are Histone Deactylase Inhibitors
This may be one of the most exciting and overlooked roles of ketones versus Alzheimer’s. A histone deacetylase inhibitor (HDAC) can promote many different roles in the body such as anti-cancer, anti-inflammatory, and anti-convulsant. The primary ketone beta-hydroxybutyrate (BHB) is an HDAC and it is important to note that unlike most HDACs made by pharmaceutical companies, BHB can easily cross the blood brain barrier.
HDAC and Depression – Major Depressive Disorder (MDD) has proven difficult to treat in roughly 1/3 of cases. HDACs are often prescribed for depression and are a proven mood stabilizer. Other pharmaceutical interventions for depression focus on the manipulation of neurotransmitter levels (serotonin, dopamine, etc), but BHB may reduce depressive symptoms by reducing brain inflammation. Pro-inflammatory cytokines (IL-1β. IL-6, and TNF-α) are significantly higher in MDD. BHB reduces IL-1β levels in the hippocampus of stressed rats and pre-administration of BHB reduces hippocampal TNF-α. Researchers believe that BHB inhibits NLRP-3, a stress (and other trigger) activated inflammasome.
HDAC and Autophagy – Johns Hopkins researchers recently published a mouse study showing that transgenic mice with the equivalent of the ApoE4 allele showed cellular differences in three important areas compared to normal cells. Gene expression of Sodium/hydrogen exchanger 6 (NHE6) was 50% lower which resulted in increased acidity in endosomes. Acidic endosomes lose their buoyancy and sink into the cell instead of shuttling about, diminishing the clearing of amyloid-beta through autophagy. The researchers also found a 50% reduction in the protein LRP1 on the surface of astrocytes. LPR1 grabs amyloid-beta from outside the astrocyte and transports it across the cell membrane to the endosome for disposal. Broad spectrum HDACs fixed all three problems. In other words, an HDAC such as the ketone beta-hydroxybutyrate is capable of reversing Alzheimer’s associate damage caused by the ApoE4 allele (the most strongly correlated genetic marker for future Alzheimer’s risk).
Ketons Promote Neurogenesis
BHB and BDNF. Brain-derived neurotrophic factors are a family of peptides and proteins involved in neurogenesis, biogenesis of mitochondria, and neuroprotection. BDNF expression was known to increase after exercise or fasting. Later studies revealed that ketones also upregulate BDNF. This is one reason scientists refer to ketosis as mimicking the fasted state.
If BDNF promotes neurogenesis and neurogenesis is the opposite of neurodegeneration….
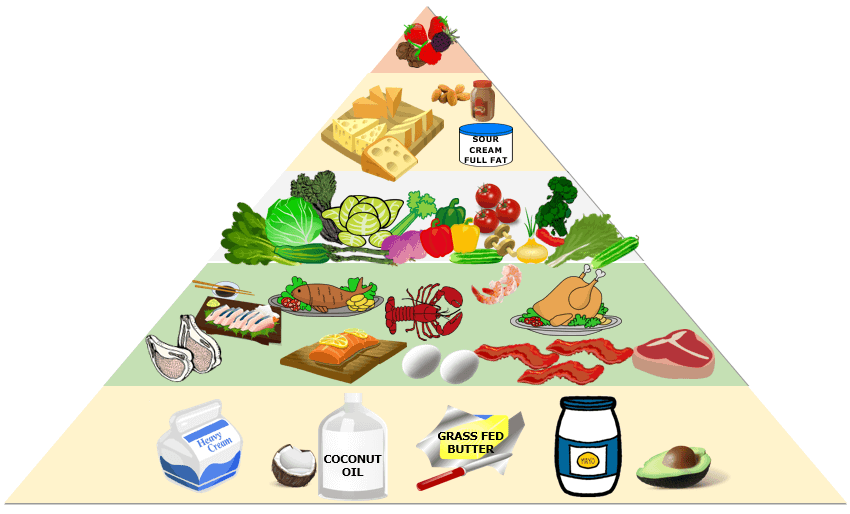
It’s Not That Hard To Do
If you are already in ketosis – congratulations! If you are interested in making the commitment there are a number of websites devoted to the topic of what to eat and not eat. There are also sites dedicated to fear mongering about ketosis, but more on that later.
Measuring ketones
One of the harder things to determine in the first few weeks is whether or not you are actually in ketosis. Here is a rundown of the three types of tests.
Urine – An inexpensive test involves peeing on a test strip and watching to see if it turns a darker color. Unfortunately, it will only work if you have extra ketones dumping into your urine (in this case acetoacetate) so if you are already thinking hard or exercising you are probably using up all the excess ketones and the test strips will not indicate that you are in ketosis (false negative).
Breath – A breath test can measure acetone levels (the gaseous byproduct of burning ketones). Sadly, a high carb intake (pizza and beer) can give a high acetone reading as gut bacteria will also produce acetone in the event of a large amount of carbs (false positive).
Blood – Beta-Hydroxybutyrate is measured with a blood test – similar to a glucose monitor. A drop of blood on a test strip is inserted into the monitor and a few seconds later you have a reading. This test is the most accurate and it measures perhaps the most important ketone body.
Scribes and Pharisees
Now a note about the naysayers and fearmongers.
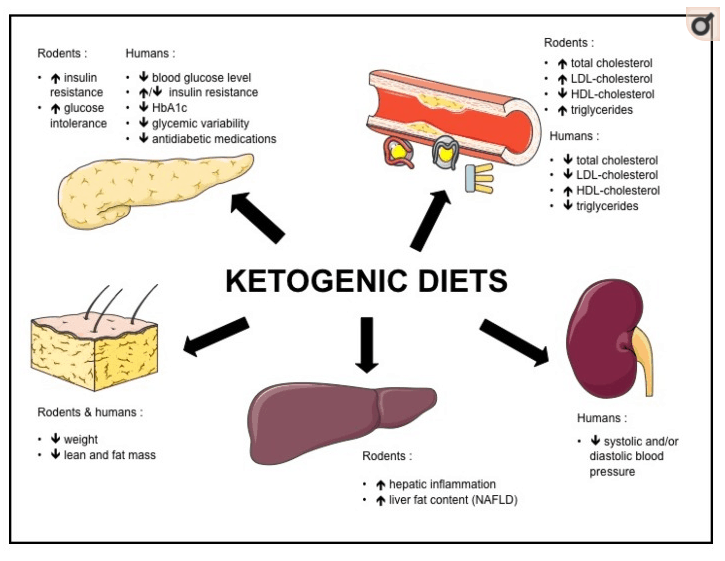
Every month sees conflicting reports over the benefits and risks of a ketogenic diet. It’s confusing, but at the heart of the matter is the difference in how rodents and humans respond to keto. For all our shared biological responses that make mouse studies so useful, keto (at least as it relates to insulin and cholesterol) may not be one. Rodents have largely opposite reactions to humans when placed on a ketogenic diet (see graphic). Therefore alarmist articles about the dangers of keto must first be considered in light of whether the alarm bells have been rung by a research team using rodents.
Image source: Nutrients May 2017
As you can see in the graphic, rodents experience insulin resistance, increased cholesterol, and non-alcoholic fatty liver disease. However, the opposite is true for humans.
Eventually rodents do experience positive benefits from ketosis especially in the brain.
Another little trap to avoid is the rodent study that sabotages the keto diet by substituting healthy fats with trans fats. I think you can see what a bad idea that would be. It would be similar to declaring all cars unsafe after taking out the seat belts and disabling the air bags.
The second most common alarmist article about keto involves maximum performance of elite athletes. The gist of the concern is that in the 24th mile of the marathon (so to speak) the athlete in ketosis just doesn’t have as much fuel in the tank. This strikes me as trivial. If that’s really someone’s reason for not following a ketogenic diet (especially if that person is not an elite athlete) then they were probably searching for an excuse.
Important update November 2018 – There is a growing body of evidence that the keto diet may be more effective for elite athletes and even elite endurance athletes. This April 2018 study being one example:
“Compared to a HC comparison group, a 12-week period of keto-adaptation and exercise training, enhanced body composition, fat oxidation during exercise, and specific measures of performance relevant to competitive endurance athletes.”
The final common criticism on the list of alarmist reasons to avoid ketosis is that the long term effects are unknown. That strikes me as odd as children and adults with epilepsy have been on long term ketosis for decades without any physical, mental, or emotional detriments attributable to a ketogenic diet.
Low Carb vs Low Fat
This is the debate that really gets the lab coats in a twist. Which diet is better for weight loss? Frankly, I don’t care. The evidence indicates that both diets will result in weight loss. So you can either eat potato chips and count your calories or you can enjoy some fat while largely ignoring your calorie intake (the keto diet results in feeling full before you can overstuff yourself).
The resolution of the debate for me lies in the fact that a ketogenic diet has many health benefits not found in the typical weight-loss diet. To put the above benefits into perspective a ketogenic diet is more effective than any known or currently-being-tested pharmaceutical at addressing the most likely factors contributing to Alzheimer’s disease such as Inflammation, Oxidative Stress, ApoE4 (namely Beta-Amyloid Deposition), Neurodegeneration, and Mitochondrial Dysfunction.
Final Thoughts
The role of depression as either a contributing factor or a symptom of Alzheimer’s is not clear, but the two are strongly correlated. And while it may be a chicken and egg sort of question it’s nice to know that a ketogenic diet can alleviate depression, even treatment-resistant depression.
And finally, a little cheat that can give you some of the benefits of ketosis right now today. Coconut oil is a medium-chain-triglyceride that travels straight to the liver and is converted to ketones without regard to glucose levels. A tablespoon a day is a nice way to help transition to ketosis before your dietary changes fully kick in and it’s a pretty good supplement in general.
A short list of other ketosis benefits (not necessarily related to Alzheimer’s)
Epilepsy; Obesity – It even results in weight loss among endurance athletes; Fatty Liver Disease; Heart Disease; High Blood Pressure; Alzheimer’s; Parkinson’s; Diabetes: Type 2; Diabetes: Type 1; Cancer.
*My apologies to Stanley Kubrick for my contrived reference in the title to Dr. Strangelove.


[…] increased production of KYNA by substantial amounts. Compared to rats fed a regular diet, the ketogenic diet resulted in an increase of KYNA concentrations in the hippocampus of 256% for young rats and 363% […]
[…] than the above mentioned Metformin at decreasing glucose and increasing insulin sensitivity. The benefits of the ketogenic diet is […]
[…] dying from lack of food for PPAR alpha to engage. In fact, PPAR alpha is a necessary component of ketogenesis where it promotes uptake, utilization, and catabolism of fatty […]
[…] to ketosis – coconut oil is a medium-chain-triglyceride and as such is converted by the liver into […]
[…] “cholesterol” so again I decline to include that. However, they also mean that one should eat better and I agree although I’m sure my list of approved foods is very different from […]